|

Lab
Diagnostic Testing: Cytology
Microscopic
examination of direct ocular specimens may provide valuable information
but depend on the quality of the sample. Smears are generally obtained
from the conjunctiva, cornea, aqueous, vitreous, and punctum. There
are many types of stains used to examine direct specimens. The gram
and giemsa stains are used in our laboratory. Gram stain is used
to examine for bacteria, and the giemsa stain is used to determine
cytology. The giemsa stain is also excellent for detecting bacteria,
fungus, and Acanthamoeba. Many laboratories are uncomfortable
with the giemsa stain because of limited experience. Laboratories
may provide the same answers with other staining techniques.
Conjunctival
specimens
Corneal
specimens
Aqueous
and vitreous specimens
Corneal specimens
The staining of corneal specimens is a valuable diagnostic tool
that can guide crucial keratitis therapy whether to pinpoint or rule out infection. The presence of bacteria,
fungus, and Acanthamoeba can commence earlier therapy. An adequate
corneal specimen is a function of the experience of the presiding
ophthalmologist. ONLY TRAINED OPHTHALMOLOGISTS SHOULD OBTAIN CORNEAL
SPECIMENS. Corneal specimens should be taken with a spatula, surgical
blade, or jeweler's forceps using a slit lamp for magnification.
When, what, and where to culture are judgement calls. In small infected
areas where the specimen may be sparse, an adequate culture is probably
more important than a smear. The complications of perforation and
denuding an intact epithelium may endanger a favorable prognosis.
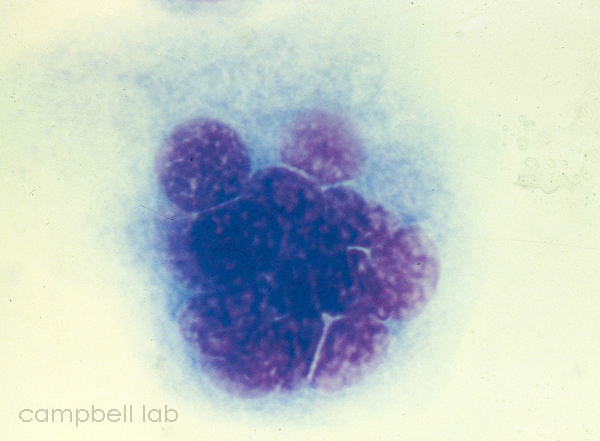
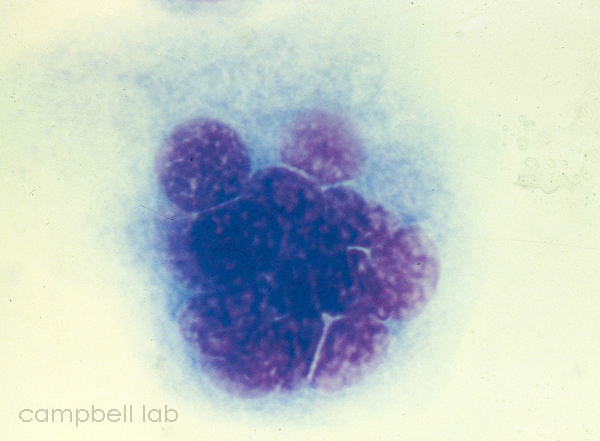
HSV multinucleated epithelial cell
(Click on image to enlarge)
 |
Aqueous
and vitreous specimens
The staining of aqueous and/or vitreous specimens is also diagnostic
in detecting the appearance of bacteria, fungi, and the inflammatory
response. ONLY TRAINED OPHTHALMOLOGISTS SHOULD OBTAIN INTRAOCULAR
SPECIMENS. Aqueous and vitreous specimens should be placed directly
on the slides from the tapping syringe and needle. The sample SHOULD
NOT be smeared over the entire slide like a blood smear. This makes
examining the slide more difficult. Slides are air-dried, fixed,
stained, and examined. Intraocular specimens awaiting transport
to the laboratory are quite stable at room temperature.
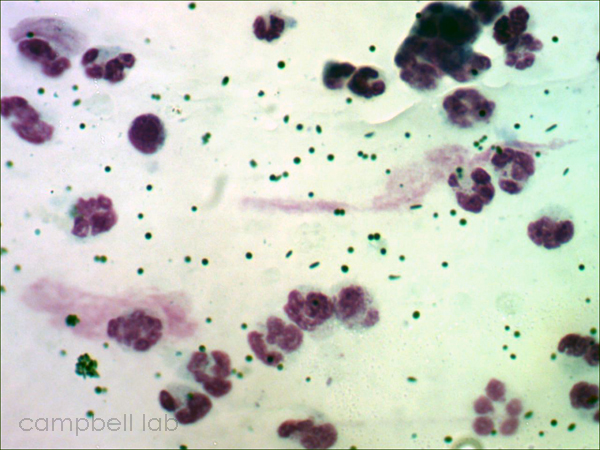
Pigment granules from vitreous
(Click on image to enlarge)
 |

|
 |

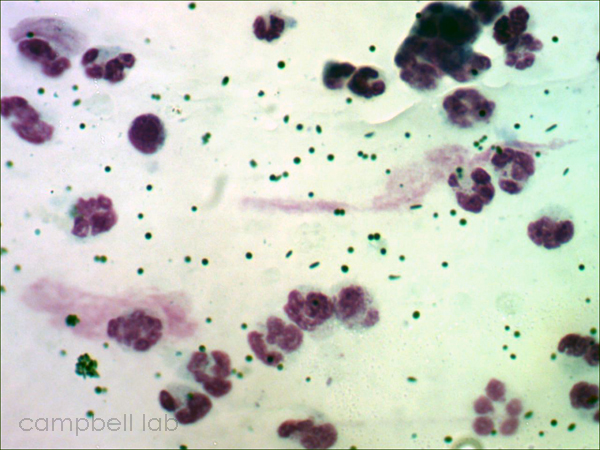
Slides for Gram and Giemsa
(Click on image to enlarge)
 |
|